"Every human being of adult years and sound mind
has a right to determine what shall be done with his own body; and
a surgeon who performs an operation without his patient's
consent commits an assault, for which he is liable in
damages."
— JUSTICE BENJAMIN CARDOZO
In medical care, informed consent is the process of communication between a physician and a patient that results in the patient's authorization or agreement to undergo a specific medical intervention. Arising from both ethics and law,1 medical informed consent is a foundation of the fiduciary relationship between a patient and a physician.
A medical consent form does not equate to medical consent. In an effort to obtain documentation of consent and evidence that they have fulfilled their legal and ethical responsibilities, health care professionals can lose sight of the important role that the informed consent process can play in their relationship with their patients. These professionals may also overlook the risk-mitigation benefits that informed consent can provide. When treated as an educational process involving an exchange of ideas, informed consent can build a sense of partnership between a physician and a patient, with shared decision-making and responsibility for outcomes.
STATUTE VERSUS COMMON LAW
The legal requirement to obtain informed consent is largely found in state law. Federal law includes requirements related to informed consent for clinical research participants. It can be codified in statutes, developed by the courts through case law (ie, common law), or both. It is important for physicians to understand the legal expectations of the state or states in which they practice and the potential ramifications if they fail to comply. There can be meaningful variation between jurisdictions. For example, some states require specific informed consent for patients who will be treated via telehealth.
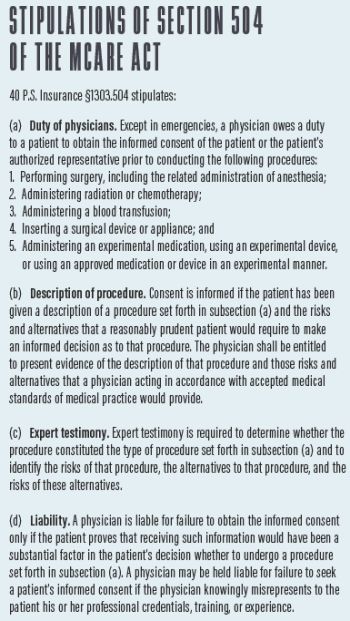
Pennsylvania provides an example of how legislation and case law interact. One section of Pennsylvania state law, specifically the Medical Care Availability and Reduction of Error (MCARE) Act passed in 2002, sets informed consent requirements and liability for a lack of adequate or obtained consent. Yet, a significant and controversial opinion of the Pennsylvania Supreme Court from 2017 is indicative of why physicians must stay informed of related case law (see Stipulations of Section 504 of the MCARE Act).
The Pennsylvania Supreme Court was called upon to determine whether a trial court erred in instructing a jury that it was permitted to consider information provided to a patient by the physician's staff members (ie, subordinates) when deciding whether consent was appropriately obtained.2 In a 4-3 vote, the Court held that, to discharge their duties under Pennsylvania's informed consent law, physicians must personally deliver information to patients and personally obtain their consent.
In finding that physicians in Pennsylvania may not rely upon subordinates to disclose the information required to obtain informed consent, the majority concluded that allowing physicians to delegate in this fashion "would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider."
A forceful dissent argued that the statute does not mandate that only physicians provide information to patients to inform their consent. The dissent also expressed practical concerns and noted the potentially negative effects of the decision. In particular, the minority raised the possibility that requiring physicians to be involved with every aspect of informing patient consent could lead to a delay in services to seriously ill patients.
CLAIMS FOUNDED ON A LACK OF INFORMED CONSENT
Medical informed consent law developed from the intentional tort of battery, which, as captured in the quote from Justice Cardozo at the outset of this article, protects individuals from an unwanted physical touching of the body by others who have neither the express nor the implied consent of the person touched.3 Battery can occur in medicine when a physician performs a treatment without the patient's consent or a procedure that is substantially different than the one for which consent was given. Battery also may be alleged in situations when a physician other than the one to whom consent was given carries out the procedure. Intent is the key difference between battery and medical malpractice, which usually is unintentional.
Most cases involving allegations of a lack of informed consent are claims of negligence, not battery. Depending on the state, noncompliance may be viewed as a presumption of negligence that may be rebutted, or it could rise to negligence per se where a statute is in place. In an ordinary negligence case, the plaintiff must prove the following:
- A duty of the physician to meet a particular standard of care;
- The physician's failure to perform that duty in accordance with the requisite standard of care; and
- A causal connection (proximate cause) between the physician's failure and the patient's injury.
The applicable standard of care can be described in different ways, including a reasonable practitioner or a reasonable person standard. Generally, physicians should imagine their duty to disclose being measured against a professional or a materiality standard. A professional standard compares the quality or completeness of a physician's informed consent against that of his or her peers, either in the community where the patient resides or nationally. A materiality standard asks whether a physician failed to provide information that a reasonable patient would consider important in making a decision.
States that have a rule, regulation, or statute that applies to informed consent and that follows a doctrine of negligence per se can make it easier for patients to recover damages because the plaintiff generally is not required to prove whether the physician's actions were reasonable. The physician's actions are assumed not to meet the standard of care if the patient can show that the physician's conduct violated the rule or statute.
DUTY TO DISCLOSE AND CONTENTS OF CONSENT FORMS
An inconsistent approach to informed consent across states can make it hard for physicians to choose a level of disclosure with confidence. What is clear is that a physician's duty to disclose risk increases as the magnitude of risk increases.
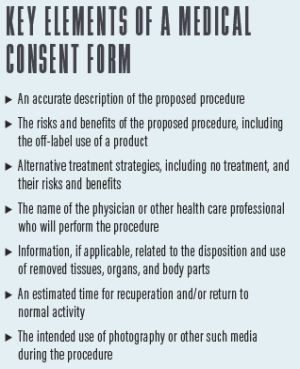
Severe risks (eg, death, paralysis, loss of cognition, loss of vision) should always be disclosed, even if the probability of occurrence is negligible. Less severe risks, if frequent in occurrence, should also be disclosed. Nominal risks that have a low probability of occurrence are less likely to be subject to disclosure. General tenets of an appropriate medical consent are found in Key Elements of a Medical Consent Form.
REDUCE YOUR RISK
Following are several tips for adhering to informed consent regulations. In assessing informed consent process and level of risk, physicians must consider whether their organization:
- Promotes the notion of informed consent as a process of effective communication between a provider and patient as opposed to just a signature on a form;
- Has a clear written policy on informed consent for care that follows state law;
- Provides formal training to physicians on effective provider-patient communication and its impact on informed consent;
- Can simplify the content, length, and language of informed consent documents and patient education materials;
- Has a process to ensure informed consent when a patient has limited language comprehension, literacy capability, or a visual or hearing impairment;
- Could enhance patient understanding through the use of decision aids, interactive media, graphical tools, or teach-back methods; and
- Ensures and documents that the physician personally participates in discussing the risk, benefits, and alternatives with the patient rather than relying exclusively on staff.
CONCLUSION
Informed consent is an essential component of the patient-physician relationship. Patients need to participate in the informed consent process to understand the risk-benefit balance for a proposed treatment strategy; physicians need to participate to ensure that patients receive adequate information and understand that they share the responsibility in decision-making.
No single approach to informed consent is risk-free. Nevertheless, the greater the attention that physicians give to the informed consent process, the less likely their patients will feel as if they were harmed by a lack of knowledge.
Footnotes
1. American Medical Association. Code of Medical Ethics Opinion 2.1.1. Accessed September 21, 2020. https://www.ama-assn.org/delivering-care/ethics/informed-consent
2. Shinal v Toms, 31 MAP 2016 (Supreme Court MD 2017).
3. Schloendorff v the Society of the New York Hospital, 211 NY 125 105 NE 92 1914 LEXIS 1028 (1914).
Originally published by Cataract & Refractive Surgery Today.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.
