Deciding whether to handle billing in-house or hire an outside billing company is an important decision for any medical practice. While it is true that not all physicians or their staffs have the experience, training and temperament to handle billing internally, it is important to understand that a billing company typically charges fees ranging from 5% to 10% of the billings/receipts they handle. This article takes a look at the benefits — and drawbacks — of outsourcing billing.
Related Read: Should You Outsource Billing?
WHAT ARE THE BENEFITS?
Billing is complicated and given the increasing complexity in the health care field, it probably will not get any simpler going forward. For your practice to handle billing internally, you need at least one skilled, well-qualified individual on your team to stay up to date with billing procedures, attend seminars regularly, and keep up on coding changes and modifiers.
Further, billing is not a learn-on-the-job endeavor — nor is it taught in medical school. The learning curve is significant and for new physician practices, there is already an overwhelming number of things to learn. To simplify practice management, you will likely need to hire an experienced billing service.
Outsourced billing can free up team members to focus on responsibilities that are more connected to your core mission of providing medical services. This, in itself, can create savings. In addition, many billing companies' coders and billers are professionally certified and know how to streamline your practice's billing processes. Having a professional, high-quality billing service that you can trust may eliminate numerous headaches and worries.
Lastly, and perhaps most importantly, specialized outsourced billing companies will accelerate your cash flow. Billing companies are able to leverage their systems and expertise to process claims faster with fewer errors, which results in quicker payment from payors for your practice.
WHAT ARE THE DRAWBACKS?
In addition to the percentage fees on all billings, most billing companies charge a set-up fee ranging from $500 to $3,000, or more. One purpose of the fee is to discourage medical practices from transferring to a competing billing company and having to pay the fee again.
In addition, a billing company contract typically locks your practice into a specific time period. In the event you become dissatisfied with the company's services during that time, it will be hard to break the contract because you will have to prove the company was not measuring up to industry standards that are not necessarily well established or stringent.
If your billing company requires payments to be sent directly to the company, instead of to your practice, it may cause your practice to lose control over your funds — even before deciding whether the billing company performs up to your expectations. It is also important to keep in mind that each medical specialty has its own billing quirks and nuanced coding. So, if you outsource your billing, check references and ensure it has experience within your specialty.
Finally, the most common complaint about billing services is that they do not chase the money. Because they are paid on a percentage basis, they tend to focus their energy and resources on handling bigger customers and bigger claims. In other words, there is a tendency to chase low-hanging fruit instead of more challenging claims.
WHAT MAKES SENSE FOR YOU?
It is a good idea to periodically compare the cost of using a billing company to the costs of having internal staff handle it — including an estimate of how much additional revenue the billing company may be able to capture versus in-house billing. Because the decision is integral to both your practice's bottom line and your personal control of the practice, it can be an emotional issue. The truth is, not all physicians or their staff have the experience, training and temperament to handle billing internally. The critical decision of whether to outsource billing should be sound and well researched to ensure that your practice thrives over time.
REVENUE CYCLE ANALYSIS: FOUR KEY METRICS
One way to help a medical practice decide between in-house or outsourced billing is to answer the following question: What are the four most important reports in your revenue cycle management? If you are unable to answer this question, you probably need to outsource billing.
Those four key metrics are:
- Days in Accounts Receivable
(A/R)
How long does it take to get your average claim paid? Most practices should fall below 50 days to get a claim paid. If your days in A/R number is greater than 50, you have a possible bottleneck somewhere in the system. The formula for days in A/R is: (Total A/R divided by gross annual charges) × 360 - A/R Report
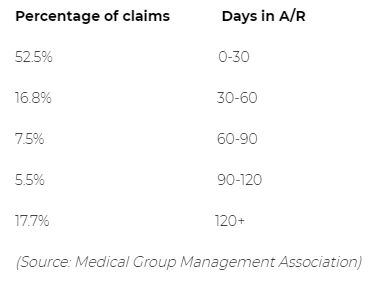
Most billing software places outstanding revenue in divided time buckets. National benchmarks that you can measure against are:
- Claim Rejection Rate
This refers to claims that have been rejected immediately by the clearinghouse on the front end. It may be because of simple demographic errors, claim data errors or a missing diagnosis, among other things. Claim rejection rates should normally be lower than 4%. - Denial Rates
Claim denials have been accepted by the clearinghouse, but have been denied by the insurance company. Claim rejection rates should be below 8%. It is important to note that 50% to 60% of all denials are never worked to adjudication, so they basically turn into lost revenue.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.

