In February 2023, the California Department of Health Care Services (DHCS) published the Medi-Cal for Kids & Teens Outreach and Education Toolkit. The Toolkit was developed to promote and improve understanding among families, providers and Medicaid managed care plans of the federal Early and Periodic Screening, Diagnostic and Treatment (EPSDT) requirement, which entitles Medicaid-enrolled children and youth from birth up to age 21 to access all medically necessary services.1
The following brief provides a summary of the Medi-Cal for Kids & Teens Outreach and Education Toolkit and considers how other states can leverage similar materials and strategies to improve knowledge and understanding of EPSDT.
Millions of Children in Medi-Cal Were Not Receiving Preventive Health Services
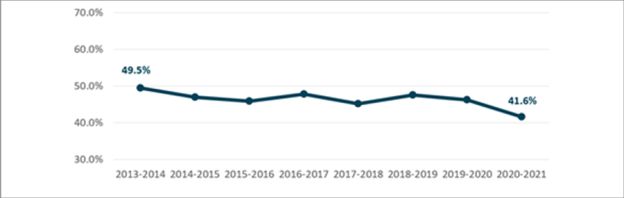
Medi-Cal (California's Medicaid) is the largest Medicaid program in the nation. Approximately 5.7 million children and youth from birth up to age 21 are enrolled in Medi-Cal, with more than two-thirds of children with Medi-Cal coverage identifying as Black or Latino/a.2 In 2019, the California state auditor released a report concluding that millions of children in California were not receiving the preventive services they were entitled to through Medi-Cal.3 The report noted that California ranked 40th nationwide for utilization of children's preventive services, or 10 percentage points below the national average.4 The low utilization rates of children's preventive health services were only exacerbated by the COVID-19 pandemic and the public health emergency (PHE), with only 23 percent of children under the age of 3 receiving a developmental screening and less than half of children being fully immunized at age 13 in 2020.5 A follow-up audit conducted in 2022 found that an average of 2.9 million children enrolled in Medi-Cal, or 55 percent, did not receive required preventive services between 2018 and 2021 (see Figure 1).6
While these trends are not unique to California—the COVID-19 pandemic caused nationwide declines and delays in access to pediatric preventive services7—reversing this trend for California's children and youth emerged as a critical priority for state leaders.
Figure 1:
Statewide Preventive Care Utilization
Rates for Children in Medi-Cal
(2013–2020)8
California's Strategy to Improve Child and Youth Access to Preventive Care
To help address and improve children's health care in California, in March 2022 DHCS published Medi-Cal's Strategy to Support Health and Opportunity for Children and Families, a forward-looking policy agenda developed across California's child-serving agencies. The Strategy focuses on addressing entrenched health inequities and identifies key initiatives to solidify health coverage for children, promote whole-child and family-based care, strengthen leadership and accountability structures, and implement evidence-based, data-driven initiatives.
A key DHCS initiative of the Strategy was to develop a toolkit focused on enhancing understanding of and access to EPSDT, including the required preventive screenings and diagnostic and treatment services.
Medi-Cal for Kids & Teens Outreach and Education Toolkit
The Medi-Cal for Kids & Teens Outreach and Education Toolkit, whose core audiences are families, providers and Medicaid managed care plans, includes three major components:
- Member-Facing Medi-Cal for Kids & Teens brochures to improve understanding of how Medi-Cal works for children, teens and young adults; what it covers; and its role in preventive care, including conducting screenings, identifying diagnoses and providing treatments. The child brochure is for children up to age 12, and the teen brochure is for youth ages 12–20.
- The Member-Facing Medi-Cal for Kids & Teens: Your Medi-Cal Rights letter to help children and youth under age 21 understand their Medi-Cal benefits and what recourse is available if medically necessary care is denied, delayed, reduced or stopped. The letter includes an overview of coverage requirements guaranteed by EPSDT and how "medically necessary services" are different for children compared to adults in Medi-Cal. It also outlines the appeals, state fair hearing and grievances processes across California's managed care and fee-for-service delivery systems.
- Standardized provider training to support Medi-Cal managed care providers working with children and youth in understanding Medi-Cal for members under age 21, including how to help children and families access medically necessary care, how to bill for covered services and whom to contact at DHCS with additional questions.
DHCS conducted extensive consumer and stakeholder review on the Toolkit to ensure the materials met the needs of children, families and providers in Medi-Cal. Based on consumer feedback, DHCS is referring to the federal EPSDT requirement as Medi-Cal for Kids & Teens in the Toolkit materials.
The brochures and the Your Medi-Cal Rights letter underwent consumer testing with parents, caregivers, teens and young adults enrolled in Medi-Cal who live across the state and speak English and/or Spanish. Overall, DHCS conducted more than 20 English and Spanish in-depth interviews and 11 English and Spanish focus groups of three to five participants. A public webinar was hosted in November 2022 to solicit comment on the member-facing materials, and additional outreach was made to dozens of consumer advocates, community-based organizations, and provider and plan associations to gather input.
The provider training was reviewed by a dozen stakeholders, including providers, managed care plans, counties and consumer advocates.
The member brochures and the Your Medi-Cal Rights letter will be mailed in summer 2023 (and annually thereafter) to the nearly 6 million children and youth up to age 21 enrolled in Medi-Cal. Starting in 2024, managed care plans will be required to deliver Medi-Cal for Kids & Teens training at least every two years to network managed care providers who work with children, teens and young adults.9 Toolkit materials are published on DHCS webpages, will be published on managed care plans' websites and are currently being translated into nearly 20 languages. For broad distribution, DHCS also shared the materials with stakeholders, providers, county offices, local health departments, non-licensed child-serving providers, schools and county departments of education, and county probation departments.
Looking Ahead
With the impact the COVID-19 pandemic has had on well-child checkup attendance, immunization rates, developmental screenings and other critical care for children in Medicaid, California's Medi-Cal for Kids & Teens Outreach and Education Toolkit can serve as a template or starting point for states seeking to emphasize the importance of preventive health care services, improve access to care and ensure providers are adequately trained on the federal EPSDT requirement.
Footnotes
1. Medicaid and the Children's Health Insurance Program (CHIP) Payment and Access Commission (MACPAC). EPSDT in Medicaid.
2. DHCS. Medi-Cal Children's Health Dashboard. March 2023. Available here.
3. California State Auditor. Millions of Children in Medi-Cal Are Not Receiving Preventive Health Services. March 2019. Available here.
4. California State Auditor. Millions of Children in Medi-Cal Are Not Receiving Preventive Health Services. March 2019. Available here.
5. DHCS. 2021 Preventive Services Report. June 2022. Available here.
6. California State Auditor. Follow-Up: Children in Medi-Cal: The Department of Health Care Services Is Still Not Doing Enough to Ensure That Children in Medi-Cal Receive Preventive Health Services. September 2022. Available here.
7. Centers for Medicare & Medicaid Services (CMS). Medicaid and CHIP and the COVID-19 Public Health Emergency. January 2022. Available here.
8. California State Auditor. Follow-Up: Children in Medi-Cal: The Department of Health Care Services Is Still Not Doing Enough to Ensure That Children in Medi-Cal Receive Preventive Health Services. September 2022. Available here.
9. DHCS. All Plan Letter 23-005: Requirements for Coverage of Early and Periodic Screening, Diagnostic and Treatment Services for Medi-Cal Members Under the Age of 21. March 2023. Available here.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.




